A little girl lost her voice just days after her illness began, yet doctors insisted it was a simple viral infection. Her parents were told to wait it out. They would later find out that a basic test could have changed everything and saved her life.
Cassie was five, energetic, and in her first year of school when she began showing signs of what doctors described as an ordinary seasonal virus. The symptoms, initially mild, didn’t raise alarms among the professionals who examined her. But for her parents, something didn’t sit right.
As Cassie’s condition steadily declined, they were left clinging to medical advice that would soon prove devastatingly wrong. No one realized that her body was fighting a bacterial infection that affects hundreds of millions of people worldwide and is often resolved with a single course of antibiotics. Little Cassie never got that chance.
Early Symptoms and a Dismissive Diagnosis
It began with a sore throat and hoarse voice, symptoms common enough in young children that they rarely cause panic. But within three days, Cassie had lost her voice completely. Her mother, Jasmine, and stepfather, Justin Sutton, grew concerned. Something felt off. Cassie wasn’t acting like herself.
Seeking answers, the family took her to a local doctor. The assessment was brief and uncomplicated. Cassie was diagnosed with a viral infection, likely a cold, and they were told to let it run its course. There was no further investigation into her symptoms.
The advice was to keep her comfortable at home. Despite following the doctor’s instructions, Cassie’s condition didn’t improve. Her energy was fading, and her voice hadn’t returned. Still, reassured by professionals, her parents held on to hope that rest and time would be enough.
Escalating Trouble and an Emergency Room Visit
As days passed, Cassie’s breathing began to change. What started as quiet fatigue turned into visible distress. Her stepfather later described it as resembling an asthma attack or the labored breath of someone with emphysema. It was clear that something more than a cold was taking hold.
Alarmed, Cassie’s parents rushed her to the emergency room. There, doctors performed tests for COVID-19 and respiratory syncytial virus (RSV), both of which came back negative. Once again, the family was told she likely had a viral infection.
Despite Cassie’s growing discomfort and difficulty breathing, they were advised to take her home and continue monitoring her. No bacterial tests were ordered, and antibiotics were not considered. Cassie was sent home for the second time, her parents still searching for answers that the system wasn’t giving them.
What Is Strep A?
What no one considered was one of the most common yet potentially dangerous infections among children her age: group A Streptococcus, more commonly known as strep A. The condition primarily affects school-aged children between five and 15, and can spread easily among siblings, caregivers, teachers, and anyone in close-contact settings.
Households, daycares, schools, colleges, and even military barracks are considered high-risk environments due to the ease of person-to-person transmission. Strep A is most known for causing strep throat, a condition that inflames the throat and tonsils — the lymph nodes at the back of the mouth.
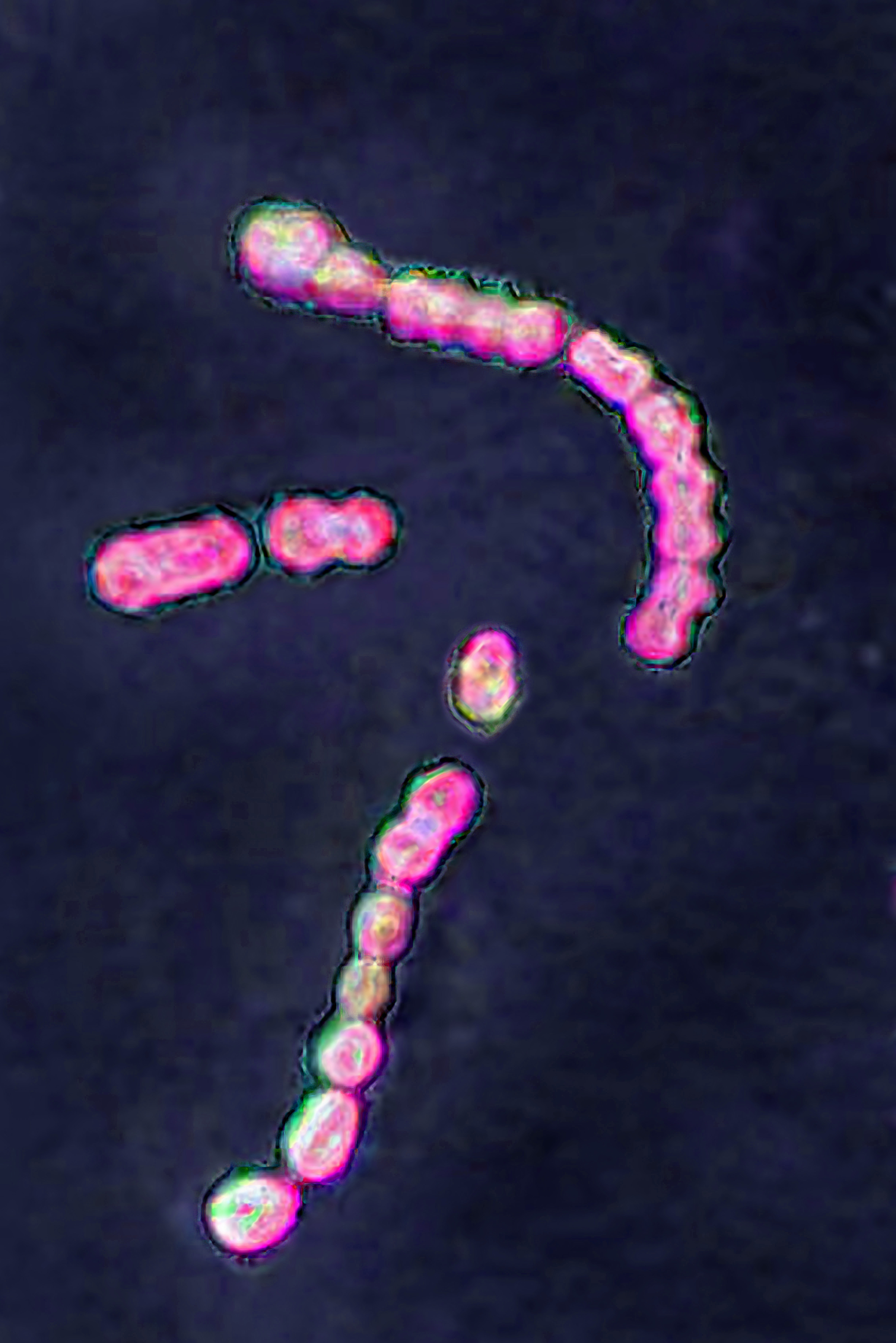
Optical microscopy image of group A Streptococcus pyogenes, the bacterium linked to strep throat and other serious infections | Source: Getty Images
Unlike typical colds, strep throat often comes with a sudden, severe sore throat, fever, and swollen lymph nodes. The inflammation typically spreads to the surrounding area, resulting in pharyngitis, or sore throat.
Diagnosis is simple. Treatment involves antibiotics, typically penicillin or amoxicillin. A quick throat swab can confirm the presence of the bacteria. For those allergic to penicillin, alternative antibiotics can be prescribed. Medication may be delivered via pills, liquid, or injection.

A medical worker takes throat swab samples from a child | Source: Getty Images
The standard treatment lasts ten days, and the full course must be completed even if symptoms improve early, to ensure the bacteria are fully eliminated. Stopping early increases the risk of complications or recurrence.
With proper diagnosis and treatment, strep throat typically resolves in seven to ten days. But when misdiagnosed, as in Cassie’s case, the delay can have irreversible consequences.
Collapse at Home and Medical Response
Despite being discharged with instructions to wait it out, Cassie’s condition did not stabilize. At home, her symptoms quickly shifted from concerning to critical. What had once been labored breathing became an emergency.
Her lips turned blue, and she started drifting in and out of consciousness while in her mother’s arms. Jasmine immediately called triple-0, and as they waited for help to arrive, Justin began CPR. He continued for ten to 15 minutes until paramedics arrived and took over.
Cassie was flown by medical helicopter to Westmead Children’s Hospital. There, doctors worked urgently to revive her. But by the time she arrived, her body had already endured too much.
A Diagnosis That Came Too Late
At Westmead Children’s Hospital, doctors did everything they could to revive Cassie. For 78 minutes, they performed continuous CPR, but the lack of oxygen had already caused irreversible damage. On August 28, 2023, her parents were called in for a meeting.
There, they received the news that Cassie had been pronounced brain dead. It was only after this that the hospital conducted a throat swab. The results confirmed what none of the earlier examinations had tested for. Cassie had contracted strep A.
The bacterial infection that had gone undetected could have been treated if caught in time. Her family was left grappling not only with the loss but with the knowledge that the condition was entirely preventable. The illness had been hiding in plain sight.
Global Prevalence and Risks
Cassie’s case is far from isolated. Group A Streptococcus is one of the most common bacterial infections worldwide, with healthcare providers globally diagnosing over 616 million new cases each year. Of those cases, around 500,000 result in death.
In the U.S., it accounts for about 15 to 35 percent of sore throat cases in children, and five to 15 percent in adults, making it one of the most common reasons children visit a doctor.
Despite its prevalence, it is frequently overlooked during initial examinations, especially when symptoms resemble those of a viral cold. Because cough is typically absent in strep A infections, the presence of fever, sore throat, and fatigue without respiratory congestion should prompt immediate testing.
Strep throat gets its name from the group A Streptococcus (GAS) bacteria that cause it. There are more than 120 strains of this bacterium, and while most cases are mild, certain strains can lead to severe complications.
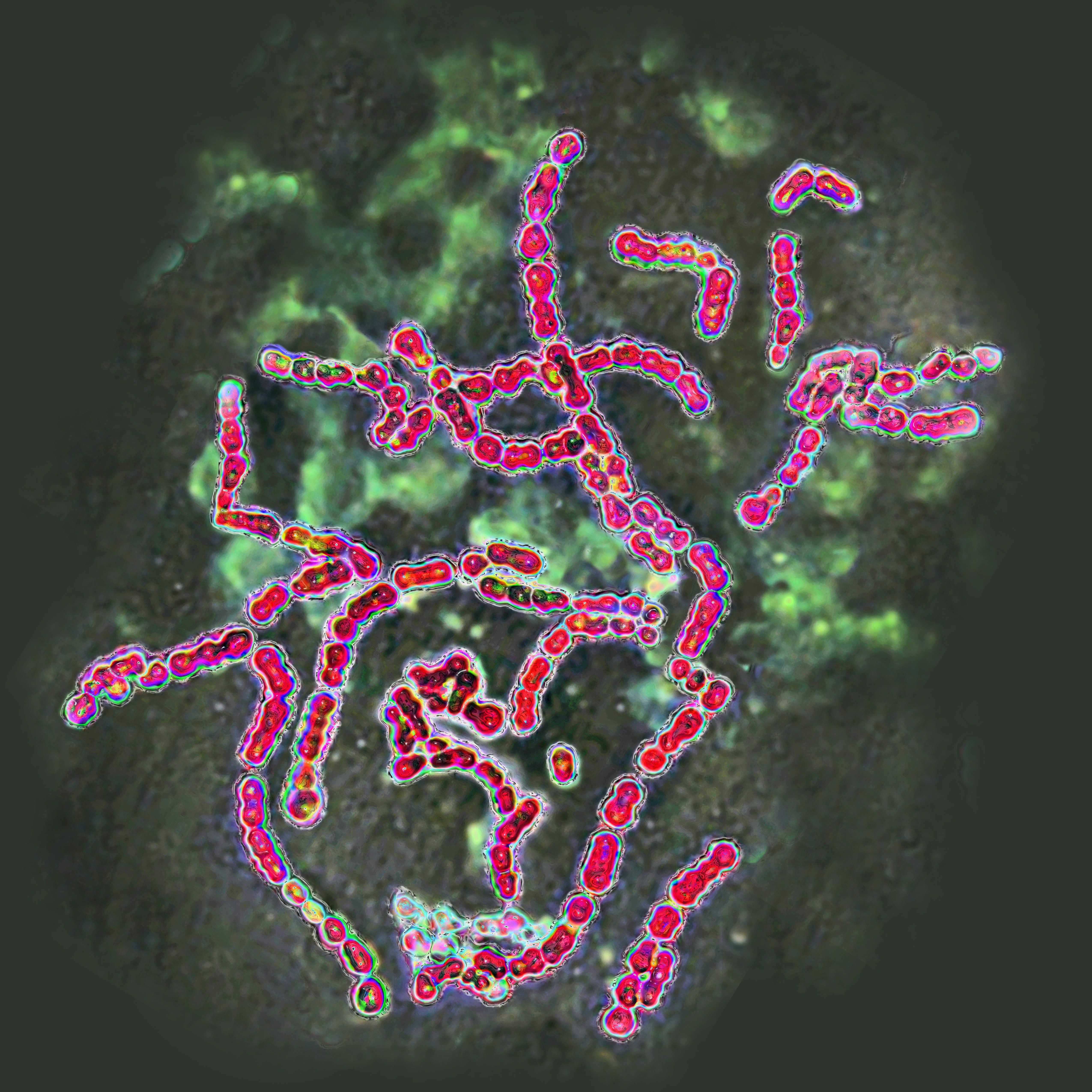
Optical microscopy image of group A Streptococcus pyogenes | Source: Getty Images
If untreated, strep throat may develop into rheumatic fever, a serious illness that can cause permanent damage to the heart and its valves. Symptoms often come on suddenly and may include:
- A severe sore throat
- Fever that spikes quickly, often on the second day
- Chills
- Headache
- Loss of appetite
- Abdominal pain
- Nausea or vomiting
Notably, a cough is not usually present with strep throat. This distinction matters: when a patient has a cough and cold-like symptoms, it’s more likely to be viral, not bacterial. However, some people infected with strep A may show no symptoms at all, making them unknowing carriers.
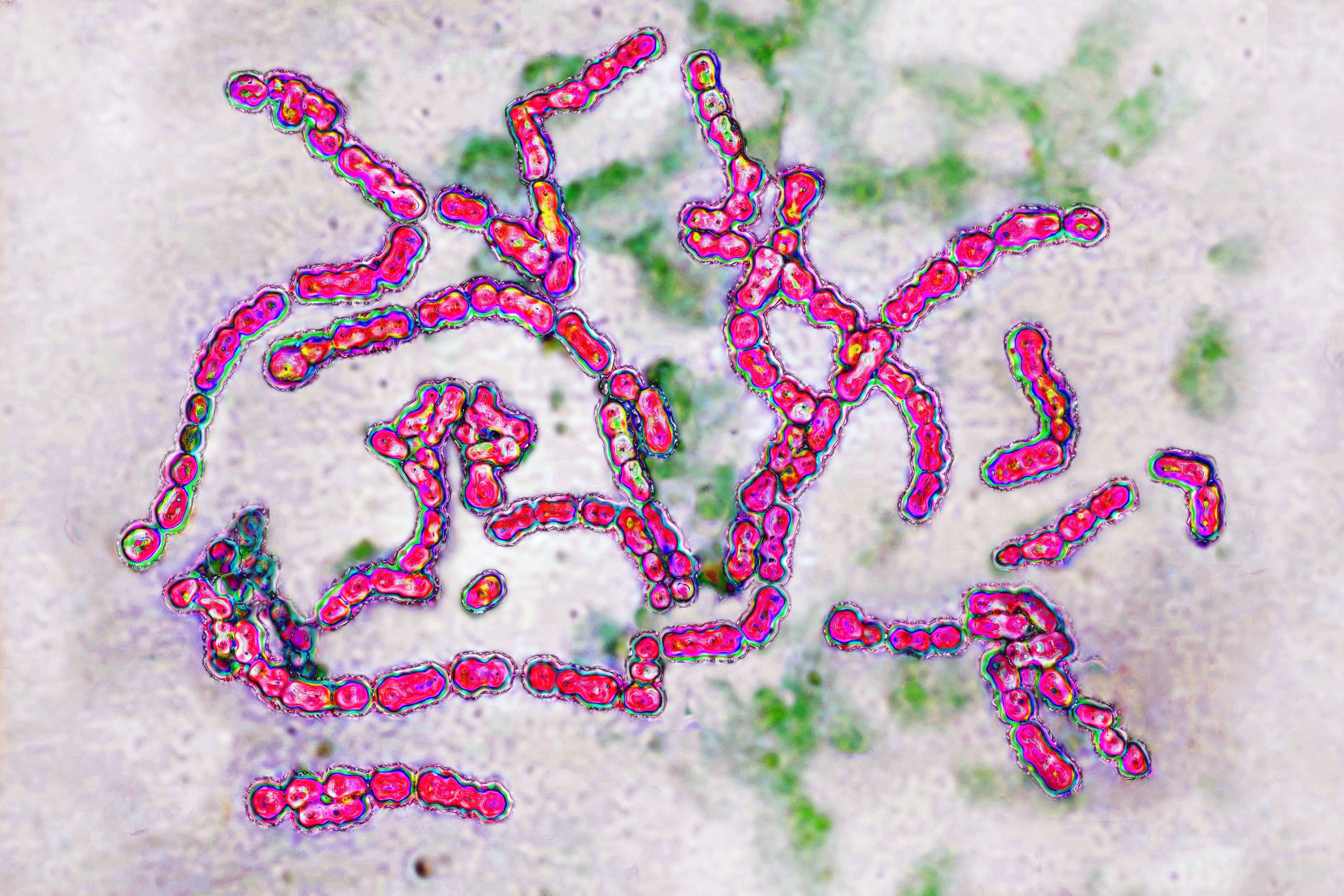
Group A Streptococcus pyogenes, the bacterium linked to strep throat and other infections | Source: Getty Images
Strep throat is highly contagious. Even those without symptoms can spread it, though people with active symptoms are more infectious. It spreads through respiratory droplets by coughing, sneezing, or even sharing utensils.
With proper diagnosis and treatment, strep throat typically resolves in seven to 10 days. But when misdiagnosed, the delay can have irreversible consequences. Yet in many cases, including Cassie’s, such testing is not performed unless specifically requested.
In children, whose immune systems are still developing, the condition can escalate with alarming speed. Awareness and timely intervention remain the most effective tools for prevention.
Cassie’s Final Gift on Jersey Day
In the days following Cassie’s passing, her family faced decisions no parent ever wants to make. Amid their grief, they chose to honor her life by helping others. Cassie’s organs were donated on September 1, 2023. The day coincided with Jersey Day, a national campaign in Australia that promotes organ and tissue donation.
Three children received life-saving transplants as a result of that decision. All three recipients were expected to make full recoveries. For Cassie’s family, knowing she was able to help others brought a sense of meaning to an otherwise senseless loss.
Her stepfather described her as a “real-life superhero,” a child who, in the face of unimaginable circumstances, was able to change the course of three other families’ lives.
Grief, Reflection, and a Plea for Awareness
As they prepared for Cassie’s funeral, her family described feeling numb, a state that allowed them to function moment to moment. In the quiet between arrangements and farewells, the weight of what had happened settled in.
While nothing could bring Cassie back, her parents found themselves returning to the same thought: the outcome could have been different. A single course of antibiotics might have saved her. The infection was treatable, and the warning signs had been there.
Still, they weren’t focused on blame. For now, their priority was making others aware. They urged families to speak up when something doesn’t feel right, to trust their instincts, and to ask for tests even when reassured by medical professionals.
“But what I’ve said to everyone is we’re going to worry about those doctors later because that’s a fight for a different day,” said Justin. Their hope now was to prevent other families from facing the same loss. Jasmine and Justin’s story is not isolated.
In the UK, another family experienced a nearly identical heartbreak when doctors dismissed the symptoms of their five-year-old daughter, just hours before she died beside her mother in her sleep.

